Meeting with Methodist
On Thursday (Feb. 25), Mitch and I met with Dr. Wells and her amazing nurse Stacey at Nebraska Cancer Specialist (NCS) at Methodist. She spent an hour and a half with us going over the MRI and biopsy results, making sure all our questions were answered. In my experience, a doctor spending an hour and a half with a patient is unheard of and I left super impressed.
Dr. Wells makes me feel like she has all the time in the world for me; nothing else matters when she comes into that room. Like she has no other patients. It’s just us in that small little treatment room making plans of attack. It’s “address Julia cancer time and we can take all the time we need to do that.”
She treats me like she is just providing all the information and I am ultimately in charge of deciding what happens. I get options. I get her opinions on those options based on what she’s seen in journals or in practice. If she is not sure she is honest about that.
She writes things down. She speaks to me with respect and understanding that I have a baseline medical knowledge, while still ensuring Mitch is following along too. I can tell she adjusts her bedside manner to make it patient specific and tailored to me. I respect and admire that in providers. I could go on and on about her and nurse Stacey but I think you warriors get the point. She ensures I have all the information I need to be the most prepared to make the best decisions for me and I’m el presidente of her fan club.
My Right Mass
Those decisions start with going over the MRI and surgical report, which honestly were quite depressing and sobering. Warriors: if you remember from our previous science lessons, MRIs give very detailed images. This detail showed a 10cm mass in my right breast…..yes, 10 centimeters. Medical knowledge-informed warriors take a moment and let that huge number sink in, then keep reading.
The rest of you, well I’ll explain that 10cm is HUGE when it comes to medicine, Donald Trump saying HUGE big. It is enormous and not great news. While this is a huge true undeniable fact, us in medicine know it’s just a number and only one puzzle piece to this much larger cancer picture. That number alone will not determine my odds or prognosis. There is a lot in medicine that is unexplainable when it comes to how patients respond to treatment and I plan on being one of those everyone says, “I’m so surprised she beat that. I didn’t think she had a chance.”
So while 10 centimeters is huge, it’s not the end and there is kind of a caveat to that number. The main mass is 7 centimeters by 7 centimeters, but there is some spider webbing of my tumor so from furthest-to-furthest point it’s 10 centimeters. While it’s terrifying to be in double-digits, it’s important to know exactly where this tumor starts and ends as it will help the surgeons get it out for sure after chemo. Like President Bush said, “no children (or tumors) left behind.” Hopefully my surgeon executes this idea better than Bush did or I’m F*CKED! (OOOOHHHH BURN!!! You damn snowflake Julia!)
Lymph Involvement
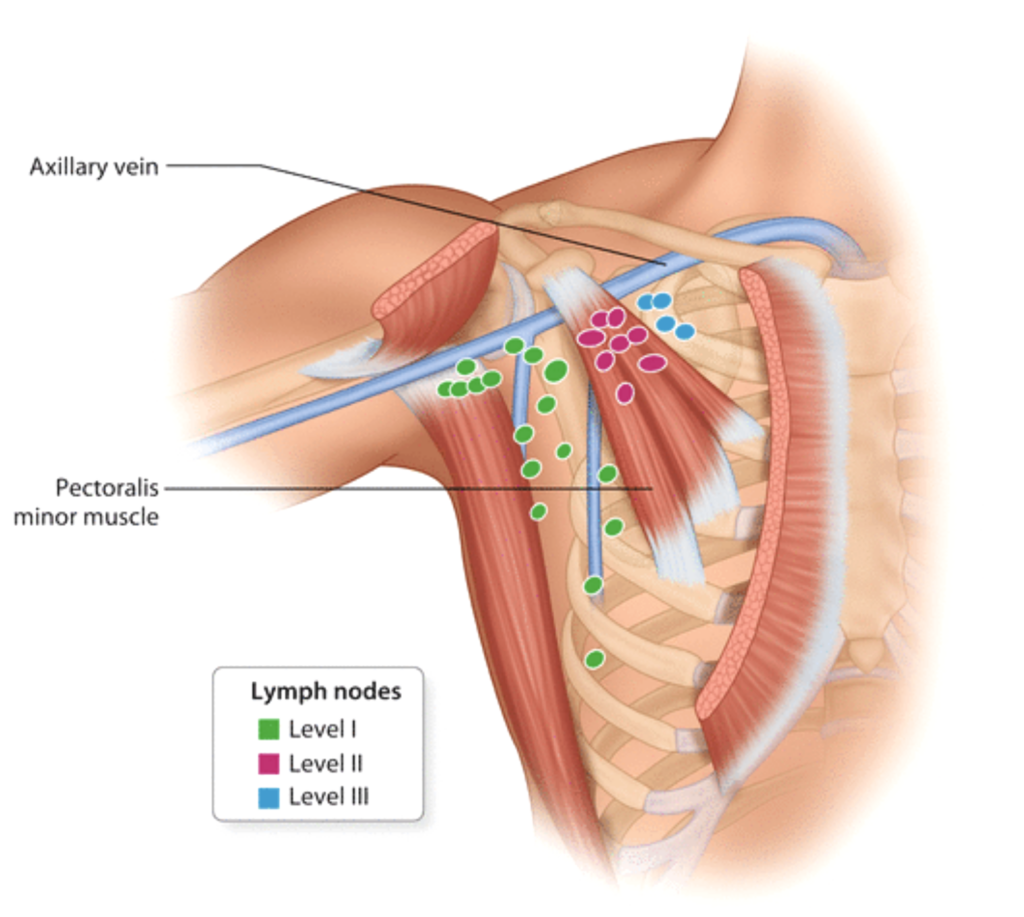
Jokes aside, 10 centimeters… right breast tumor… Good news is the tumor does not invade my chest wall. It’s knocking on its door, but has not invaded it. Bad news is there is lymph node involvement. There are three levels of lymph nodes based on the nodes proximity to the surface. Of course I have cancer at all three levels, as deep as it can go. This means I will have to have a pretty radical mastectomy after chemo and my chances of lymphedema are increased.
Lymphedema is when the lymphs are blocked and can’t drain. This increases infection risk and is a very bad side effect I am most worried about and hope I don’t ever have to deal with. I say “ever” because it’s a side effect I’ll have to watch for forever after my mastectomy. Cancer is the gift that never stops giving!
My Left Mass
Speaking of cancer always giving, another super awesome and totally not worrisome finding on my MRI was in my left breast. There is a 1 cm mass or possible lesion in my left breast. They can’t tell on imaging if the tumor is the same cancer as in the right breast, a new different cancer, a benign cancer, or something else completely. It is there and a new fun issue to deal with! How? We will get to that in Step 4 below.. Like a terrible stalker ex, my cancer just keeps giving me gifts I most certainly do not want. Find a new woman cancer! I’m married!!!!!!!
Biopsy Results
Moving on, the next information we received was the biopsy results. These were not surprising. We had discussed these over the phone already and touched on them in the last blog post. The biopsy showed cancer in the right breast tissue sample taken, in the right lymph node sample, and not in the left lymph node sample. Don’t get overly excited, Warriors, thinking this means my left breast mass is in the clear; the sample taken was of the lymph node and not of the mass seen on the MRI. The biopsy confirms that the left lymph node that had previously been inflamed on the PET scan was due to the COVID vaccine and not cancer.
The cancer they did find (in the right breast) is identified as an invasive ductal carcinoma. This is the most common type of breast cancer, accounting for 80% of breast cancers. Now you’re most likely confused, because I had said it was inflammatory cancer. Well I’m confused too. So are a few doctors. We will circle back to that in the So Is It Inflammatory? section, so just put that aside for now while we finish the biopsy results.
Results of Tumor Type
The other aspects of the results were the estrogen (ER), progesterone (PR), HER2, and Ki-67 statuses. As you learned with me in prior blog posts my tumor is ER very positive, PR a little positive, and HER2 negative. If you thought you were getting lucky without a science lesson today you were wrong! I can’t help myself! It’ll be a quick one though!
Science Lesson Intermission
The way they decide how positive or negative tumor receptors are is by doing a nuclei stain. This is when part of the tumor is put on a microscope slide, then stained to show the cells (or nuclei) that have positive or negative receptors present under the microscope. My tumor had 91% of the nuclei receptive to estrogen, making it very estrogen positive. It showed 2% of the nuclei stained receptive to progesterone, meaning low positive. It showed 0% HER2, hence the negative results. It also showed that 58% of the Ki-67 stain was positive.
Ki-67 is assessing the cell division. If a cell divides fast, it has a high Ki-67 score. If a cell divides slow, it has a low Ki-67 score. In biology, division means “duplicates” or “make more of.” To recap (at least in theory), a high Ki-67 score means the cancer grows fast. Low Ki-67 score means the cancer grows slowly.
Anything over 25% of cells positive on the slides is considered a high score. My cancer had a high Ki-67 score at 58%, meaning it grows fast. This is not all bad scary news, as again in theory, cancer that divides or grows fast is typically more responsive to chemo, meaning my cancer should respond well to chemotherapy and shrink the tumor size.
Back to Scheduled Visit Recap
That was pretty much it from our visit. We did discuss prognosis but there aren’t any good tools right now to give a very accurate prognosis percentage. The only tool that exists puts my ten year survival rate at around 40 percent. This tool is outdated and does not take into account some of the treatments I’ll be doing or some newer data out there. Most newer studies (which take into account all the treatment options given) are showing 60-70% ten year survival rates. You decide what you want to believe in that regard.
Personally, I believe, percentages don’t mean sh*t except when super low or high across the board. To me, I’m in a gray area. Odds aren’t totally against me, but aren’t giving me the all clear warm fuzzies either. It’s all going to come down to how my body and cancer respond to treatment, which I have little control over. I’m going to give it my best shot. I’m doing my best to be as healthy as possible, put all the positive vibes out into the universe, and believe in science and myself that I can beat this.
So Here We Are
Warriors, I’m not going to lie to you, this has been very hard to revisit and write out. I am sitting here listening to a Spotify playlist based on my love of Snoop Dogg, just shaking my head, throwing my fists in the air, doing finger guns at the report, and taking a lot more breaks than I normally do in my writing.
It’s so much to take in. Re-reading it is reinforcing how real this is. How big of an obstacle this is. What I am really up against. Sometimes it sucks to have this medical background and knowledge, because I understand the severity of this situation a lot more than I would like right now.
Warriors, do you hear that whining off in the distance? It’s our foster acceptance wanting attention! Listen you little cutie acceptance I am glad I have this information. I am glad I have the medical knowledge and understand this. I just wish I was not in this situation! It’s bullsh*t. Oh hey there grief! Didn’t see you lurking there! F*cking cancer fosters. Ya’ll the worst. Katie, can you please come and take them back already!!! (Oh, if only it was that easy)
A Second Opinion
When they found out I had cancer, one thing a lot of people very close to me were adamant about was to get a second opinion. This seemed absolutely ridiculous to me. There are very specific standards of care. A standard of care means: if someone has issue ABC, then XYZ should be performed no matter what hospital the patient presents to. There should be no difference in the treatment the patient receives.
Standards of care is what made me think this was an absolute waste of my time, but I agreed to do it anyway. On Friday (Feb. 26), we went to the Nebraska Medicine Breast Clinic (NMBC) at Village Pointe to see Dr. Reed with Oncology and Dr. Santamaria with Surgery. After figuring out which building we were supposed to be in, the first thing that both Mitch and I were impressed with was the building itself: it was shiny, new and beautiful. It did not give off the depressing vibe that the outdated Nebraska Cancer Specialist suite gave at Methodist. It also appeared to be much smaller of a clinic and less busy. There was no one in the lobby when we came or left.
Step 1: Meet the Medical Assistant
Visits always start with the medical assistant who does the vitals and checks that everything has stayed the same since the last visit. She was not as personable as the medical assistant at Nebraska Cancer Specialist. She did her job very well. I just felt like another patient to her and not a person.
Step 2: Meet the Oncologist
Dr. Reed was next. She examined me and then explained that she would use a similar treatment as Dr. Wells at NCS with one potential difference. She would use a drug called a PARP inhibitor, a drug used to treat only BRCA2 cancers and is typically given post surgery in breast cancer patients. It is not yet approved to treat BRCA2 breast cancer while on chemo, but the study she saw published just a week ago shows giving it at the same time as chemo increases survival chances in BRCA2-positive breast cancers. She said she wasn’t 100% sure of when they gave it during chemo, just that she was pretty sure it was given during chemo. She said she would want to follow these trial protocols and needed time to look it up, but is willing to go all way up to the Nebraska Insurance Board to get the approval needed to take the drug at the same time as chemo.
That was a new option I wasn’t prepared to hear! and was now confused on which doctor to go with! My confusion aside, Dr. Reed was very impressive and knowledgeable. But I felt a little rushed: I could tell she had other patients to talk to and wanted to stay on schedule. She didn’t have an hour and a half like Dr. Wells did and didn’t have extra time to spend with me. I wasn’t her only patient and I felt that.
Step 3: Meet the Surgeon
Up next was Dr. Santamaria with Surgical Oncology. First, he examined me and then requested we head down the hall so he could do his own ultrasounds to view my tumors himself. I thought this was very impressive and “Grey’s Anatomy” worthy. In my experience, most surgeons don’t take the time to perform the ultrasound themselves and if they do, it’s while the patient’s actually on the table and ready to be operated on, not prior to. Santamaria explained he wanted to see for himself what he was dealing with, rather than trust another person’s readings. Again, color me impressed.

(It’s that black circle. That’s the left breast tumor)
Step 4: Discuss Treatment & Surgery Options
After that we went back to the room to discuss options. His mastectomy plan was pretty similar to what Dr. Kolkman (NCS) had suggested, but again with a caveat. NMBC has a plastic surgeon, Dr. Figy, who can do lymph node transplants, a super new and specialized surgery. Dr. Figy can either transplant my own lymph nodes into my arm or work with my blood vessels to make armpit lymph nodes that connect with my lower arm lymph nodes to drain properly. This would greatly decrease my chances of lymphedema in the future. I am 100% on board with this plan, and fully plan on using Dr. Santamaria and Dr. Figy for my mastectomy. 100 percent hands down, no questions asked, it’s them.
That choice figured out, here’s where it all gets interesting and confusing. First off, Dr. Santamaria and Dr. Reed felt strongly that we should get a biopsy of the left side mass to ensure the left side isn’t a different type of cancer. If the left side is a HER2 positive cancer, it would change my chemo options because we would have to add a drug to fight off the HER2 receptors in addition to the rest of my chemos and drugs. I feel like this is reasonable and agreed to do that biopsy with NMBC on Monday.
So Is It Inflammatory?
The second and more interesting factor is that Dr. Santamaria and Dr. Reed both feel like my breast cancer is not inflammatory. The reasoning behind that idea is because the only way to diagnose inflammatory breast cancer is by how it clinically appears on the patient at the time of diagnosis. The breast must appear large, warm to the touch, and with redness or “orange peel” look taking over at least one third of the breast. When I first visited with Dr. Kolkman in early February, my right breast had that similar appearance. Since I stopped taking my hormones for my endometriosis, my breast no longer looks like this. It’s still different in size, but the redness and warmth has reduced significantly. I also never had the orange peel look either. If I had presented today, no doctor would have called it inflammatory breast cancer.
They also stated that ER/PR/HER2/Ki-67 statuses don’t make sense with an inflammatory breast cancer presentation. I can’t remember what about it in particular didn’t make sense but they were really held up on that. It really doesn’t make a difference to me though.
Inflammatory or not it does not change any of my treatment plans except for my mastectomy. If it is inflammatory breast cancer, we would take more breast skin to ensure it’s all gone. If it’s not inflammatory, we could leave more skin intact. It is not a huge difference in care, it is just very confusing and interesting. Am I a zebra with a weird ER/PR/HER2/Ki-67 status and inflammatory cancer? Is it not inflammatory cancer? Did the COVID shot affect my presentation? There is really no way to ever know the answer to these questions and it doesn’t really matter. Santamaria said he’d take more skin if I felt more comfortable with that. It’s just interesting that my cancer first presented as inflammatory and now it’s not. It’s rare and confusing, which I felt like NMBC as a whole was very distracted by.
Step 5: Meet the Nurse Case Manager
After all that we met the nurse case manager for Dr. Reed, who was nice, very knowledgeable, and spent a lot of time with us. But I didn’t feel like I really clicked with her. I felt like she really dumbed things down for us and didn’t respect my medical background even after I told her I was a nurse. She also showed us the chemo rooms which are different from NCS. At NMBC, each chemo patient gets their own room for treatment. While I’m sure some patients appreciate this and enjoy looking out the window (and maybe I would too after treatment is over), it seemed so depressing to me right now. Patients are not allowed to have anyone with them during chemo anymore due to COVID, so you’re just alone in this little room with the door closed because again thanks COVID!! The little rooms felt like I’d be in a chemo jail. NO THANK YOU!
We left and got home with a lot on our minds. What now? Who do we choose for oncology? I was over it. Mitch was over it. And we got great surprises all evening long from so many of you to take our minds off everything, so thank you all. You know who you are and I’ll shout you out at a later date.
Post-Meeting Call with Dr. Wells
Even though I was over it, Dr. Wells had mentioned to call her if NMBC doctors suggested different treatments. So I did. She called me back at 3:30 pm and said she couldn’t find the study that Dr. Reed (who trained her) was talking about. She found a press release from Astrazeneca about it, but not a published study. This is important information because Astrazeneca can publish press releases on whatever information they want and they don’t have to include the bad aspects. Because it’s a press release, there is almost no way insurance will ever approve it and, personally, I’m not doing a treatment based on a press release and not a real study. It left a bit of a sour taste in my mouth for Dr. Reed, as I felt she didn’t give me all the accurate information. Dr. Wells said we would still do the PARP drug just after surgery, which seems reasonable to me.
I also informed Dr. Wells about the biopsy and she said that was totally reasonable. She said that if it was HER2 positive, she would still do red devil chemo (Adriamycin) followed by Paclitaxel with a HER2 drug at the same time. Cross that bridge if/when we get there and it shouldn’t put a delay on starting treatment, as she would still treat with red devil first anyway.
Last Call of the Day
At this point, Mitch and I were so over it and done. We agreed to sleep on it before deciding who to go with for oncology. So I took all the meds for my endometriosis pain (because for the first time in ten years I’m officially on a period), and went to bed to watch TV and chill at 5:00 pm. I figured no doctors call after 5 pm, so I was fine to take narcotics right? WRONG!!! OH SO VERY WRONG!!! At 6:00 pm Dr. Reed called me. I was half asleep when she called and had to really pull it together to talk to her. I felt like I was on the Bachelorette with all these doctors fighting over me! Everyone wants a piece of this and I still got it y’all! ??
Dr. Reed said that she had time to look more at that study she noted earlier, and realized it indeed was a press release and not a study, so we couldn’t do the PARP while on chemo. She just wanted to clarify that. I asked her how she would treat the left tumor if it was HER2 positive. I think she said she would cut the amount of AC I got, then do Paclitaxel, followed by a HER2 drug. I wasn’t a huge fan of this idea because my tumor is you know, if you remember, TEN FREAKING CENTIMETERS!
At this point, I felt like Dr. Wells had called Dr. Reed and said, “what the heck are you telling my patients and what the heck are you doing?” I can’t prove this theory and won’t even if I do ask at my next appointment, but that’s how I feel. I went to bed feeling like for NMBC I’m just another case and number, whereas for Nebraska Cancer Specialist I’m a real person. NCS treats me like they are treating a friend or loved one. To be fair, when I’m at work I also have a tendency to treat people like cases and numbers, and not like family. For me, it’s a coping mechanism to give myself space between personal and professional life. It makes me feel a bit inadequate as a nurse that I can’t make people feel as important as Dr. Wells and her team, but it doesn’t affect the care provided, just an area for me to improve on when I get back to work someday.
Now I Kindly Ask…

After sleeping I woke up with those same feelings. The treatment plan for chemo is not different with either provider. The surgery is very different. With that being said, I present to you and hope (I already know) that Dr. Mary Huerter Wells, MD, will accept this rose and be my oncologist, and Dr. Juan Santamaria, MD, (along with Dr. Sean C. Figy, MD) will accept this rose and be my surgeon.
I made this decision because I feel like Dr. Wells has a better plan in place to treat any side effects, I like how she presents everything, and I connect better with her whole team. I picked Dr. Santamaria and Dr. Figy because they can offer me lymph node replacement which greatly reduces one of my biggest fears, lymphedema.
Warriors, that it is for today. It was a lot. Imagine how I felt with all of it over the last two days! But you did it and read this far. I did it and we all are still here kicking. As always, stay magical and we will see what next week brings!
What an exhausting few days. All the information to process, worry, concentration, decisions and personalities to figure out. What if you weren’t a nurse, didn’t do your own research, etc. I always research the doctors also. My husband always asks where they went to undergrad and medical school, interned and where they ranked in their class. Really, he does every time. Sometimes get strange looks from the doctors. It’s a two way street.
Also totally understand the endometriosis problem. Fought that battle twice and finally won after a total hysterectomy at 34.
You are in my prayers. Keep the faith.
Thank you so! You’ve been such a greyt support!
I think research is calming for me too. A coping mechanism. The more I understand the better.
Great decision Julia! Go fight! We’re cheering for you ❤️
Again, a very informative and interesting read. You have such a wonderful style of writing, Julia. You make reading it enjoyable, hopeful but factual. Thank you so much for sharing this personal journey with others.
Sounds like you have your hands full over the last few days.
Don’t forget to take your me time and make sure you do it every day
Hang in there and you will succeed.
Wow … I’ve learned a lot about my own breast cancer just by reading your blog posts! You do a great job of explaining everything, which is a good way to help yourself digest the information. You would make a great case manager! In the end, you want to choose the doctors that you feel most comfortable with because you will spend a lot of time with them and (mostly) their staff. The fact that Dr. Wells trained under Dr. Reed gives you the best of both by choosing Dr. Wells. FWIW, I agree about being in a little infusion room by yourself. I had some great conversations with other patients while I was getting chemo. I was usually the youngest one there; but some of the sweet old ladies had the best perspectives on our shared journey.
You got this! Proud to be one of your warriors. 🙂
Thank you so!! I’m glad I could help another with my writting.
I’m looking forward to all the little old ladies! They are my favorite! I joke I’m gonna come out watching Wheel of Fortune again and knitting.